Pressure sore prevention is best
Pressure sore prevention is better than resolving a sore. Firstly, the story of how I acquired my first pressure sore.
After feeling bad and hearing a sound that reminded me of running water inside my body, I transferred to my shower chair and spent time over the toilet. I either had gastroenteritis or food poisoning, which is difficult for a person who cannot rush to the toilet quickly (and bad for the person who helps clean up the mess). An hour later I was exhausted, dehydrated and nauseous, and called for an ambulance. Madie helped me to quickly shower, get back onto the bed and ready for the paramedics. They agreed the best course of action was to take me to the hospital. They placed their stretcher next to my bed, and I moved across, and they secured the seatbelts to keep me in place. About 30 minutes later I transferred to the hospital bed, and one of the paramedics mentioned ‘So that is where the seat belt is’. As I felt terrible I didn’t have the ability to think about their statement.

A few days later a nurse mentioned ‘your bottom looks red’ and they moved my body to one side, and I assumed it was due to being in bed for a few days. The day after I was discharged, I felt a large and hard object on the left bum cheek. Only then I connected the words of the paramedic and nurse and realised the damage was caused by the seatbelt in the ambulance. For the next week and a half, I rubbed sorbolene cream and anti-septic ointment at various times on the area and called for a locum to visit me at home. He verified that the area wasn’t infected, and I should contact the RDNS (Royal District Nursing Service) to have treatment.
RDNS visits commence
Fortunately, the RDNS visited the next day and suggested the pressure sore be treated with regular dressings, and to reduce pressure on the area. Unfortunately, the area was directly under the boney part of the bum, and I needed to spend time lying on my right side. I cancelled all of my water therapies for the next few weeks, as well as other events, and spent up to six hours each day reducing the pressure on the damage. Although I could not feel it, the pressure sore was a pain in the bum, but I didn’t want the issue to get worse.
My sleeping routine changed as I wore underwear to bed, which helped to keep the dressing attached to my skin. I kept the undies on while transferring to my shower chair, to prevent it from being dislodged during the transfer. This presented a problem, as I couldn’t remove them once I was seated. I cut them off with scissors, which gave me a chance to dispose of my ‘Holy’ undies (the old ones with holes that males don’t want to throw away). After cutting each side, I would stretch one side of the undies and place it in my mouth, and then push down on the shower chair arms, lifting my body in the air, while the undies would fling me in the face.
Not nice, as I’ve been wearing them for a few days. During showering, I am careful not to place too much water near on the dressing, and I transfer back to bed. The RDNS nurse would visit, remove the old dressing, give the wound a clean with sterile water, remove any dead skin, take a photo (to record progress) and place a new dressing. The routine is working but may take many weeks until the skin is repaired, possibly up to twelve weeks. Or more!
If the regular dressings are unsuccessful, then barrier cream would be attempted. They provide a physical barrier between the skin and clothing, and there was always the option of being admitted to a hospital, although this course of action is usually only done when the pressure sore is rated at three or four.
What is a pressure sore?
In a few months, I will have my 9th anniversary of acquiring a disability and have avoided pressure sores until now. According to Wikipedia, a pressure sores …
‘are localised damage to the skin and/or underlying tissue that usually occur over a bony prominence as a result of pressure or pressure in combination with shear and/or friction. The most common sites are the skin overlying the sacrum, coccyx, heels or the hips, but other sites such as the elbows, knees, ankles, back of shoulders, or the back of the cranium can be affected.
Pressure ulcers occur due to pressure applied to soft tissue resulting in wholly or partially obstructed blood flow to the soft tissue. Shear is also a cause, as it can pull on blood vessels that feed the skin. Pressure ulcers most commonly develop in individuals who are not moving about, such as those being bedridden or confined to a wheelchair’.
Stages of pressure sores.
- Mild – only affect the upper layer of skin (minutes to hours to heal)
- Blister or open wound – the skin is broken and below the surface of the skin (three days to three weeks to heal)
- Crater or bad odour – dead tissue may need to be removed, and infection may require antibiotics to treat (one to four months to heal)
- Deep and big – skin is black and looks infected, and it is possible to see tendons, muscles, and bone ( three months to years to heal)
I could not imagine what it would be like to have an ongoing pressure sore for years. Once again I have to repeat – pressure sore prevention is better!
Pressure sore prevention
Many of my friends in wheelchairs have experienced pressure sores, and some have spent months in a hospital including plastic surgery to resolve the issue. I believe being overweight (thick skinned) and hairy (protects the skin) may have helped me to avoid sores, but the training during rehabilitation, as well as the advice of my partner, Madie, has been the real reason. There are many many methods of pressure sore prevention.
- Changing the seating position on a regular basis. Madie would regularly tell me to lift my bottom, and I would raise my body above the wheelchair cushion for as long as possible, and slightly change my seating position. Depending on how long I’ve been sitting, and whether there was sufficient privacy, Madie would massage my bottom while I was in the air. So often I would notice people in wheelchairs ignoring this avenue of pressure sore prevention.
- Equipment. Everything I sit on is designed to treat my body well.
- Bed Mattress – the foam is designed to reduce pressure on my body, with the outside of the mattress is firmer to help with transfers

- Medical Sheepskins – they have a very high wool density that distributes weight and pressure over a large area and can absorb moisture away from the skin, as well as reduce friction and skin tearing
- Wheelchair Cushions – the foam helps reduce pressure on my body on both my power, manual and shower chairs
- Powerchair reclining function – it relieves pressure on my bottom (as well as reducing pain in my back)
- Bed Mattress – the foam is designed to reduce pressure on my body, with the outside of the mattress is firmer to help with transfers
- Clothing. I tend to wear tracksuit pants 99% of the time, as getting dressed is quick and easy, and they stretch and are gentle on my skin. Best to avoid back pockets, or to remove them entirely. No one will see them. The best underwear is cotton rich and holds the boys in place.
- Diet. A proper diet can help the skin including high in Vitamin C and protein.
- Checks. Regular checking of my skin is vital, as I don’t have sensation below my chest. This is achieved visually, either myself or another person, and I also spend time feeling areas of my skin, such as my bottom.
These are the minimum steps for pressure sore prevention for people in wheelchairs. Can you think of more?
My complaint to SA Ambulance
As soon as I was aware of the issue, and what caused it, I emailed the ambulance service and registered my complaint, and asked what they would do to ensure this kind of problem doesn’t happen again. Pressure sore prevention should be one of their goals during transportation in their ambulances. I made mention of my lawyers, as the issue is affecting my life and caused by their service. Their response indicated it may take up to 35 days for an answer. The invoice for the ambulance arrived, asking for $999, and fortunately, I have private health insurance, and they cover the entire amount. However, I decided that I wouldn’t get the invoice paid until the complaint was resolved and my bottom was healed. Why should I pay for a faulty service? I wouldn’t pay a plumber if the tap continued to leak, so why should I pay for transport to the hospital when it damaged my body?
Time passes
6 week in. The RDNS suggests we continue placing dressings on the wound. The issue had big impacts on my life, including physical and mental health. Accustomed to swimming twice a week and weight sessions up to three times a week, I lost a great deal of physical fitness, and felt tired and had trouble sleeping. Exercise during the day sends me to sleep at night time. As I spent an extra 6-8 hours a day in bed, attempting to rest on my right-hand side, My neck, arm and wrist became sore. I felt depressed, as I cancelled the majority of my appointments, including social outings. There were feelings of anxiety, as I researched the worst case scenarios, and imagined having to spend months in the hospital.
8 weeks in. The dressings continue and I visited my dentist relating to sore gums. She discovered an ulcer in my mouth and explained that gums are affected by stress. The sore gums, as well as cold sores, commenced just after the RDNS discovered that the wound was weeping. Still no reply from SA Ambulance. I updated my complaint to include the care during my time in the hospital. The staff should have been more concerned with the pressure sore, including describing it to me, rather than just mentioning ‘your bottom looks red’.
9 weeks in. I received an email from SA Ambulance and it included an apology from the paramedics. Good to get an apology, and I had already forgiven the paramedics. They perform an important role and do it well. My complaint was focused on ensuring a similar incident is avoided. The email reassured me that patients are required to be safely secured prior to transport and this has been reinforced with the attending paramedics. It informed me that the matter has been fully investigated and the matter has been closed. I’ve been affected by poor investigations by SA Health, and I was displeased with the response and investigation by SA Ambulance.
1) My original complaint asked the question ‘What can you do to ensure this doesn’t happen again?’, and only the two paramedics were involved in the solution to my complaint. There needs to be an inclusion in the training of paramedics to adequately care for patients with paralysis, including pressure sore prevention.
2) The email suggested I should contact the SA Health consumer advisor if I required more information. I felt this was a ‘please do not contact us about this matter again’.
3) There was little concern about the ongoing healing and treatment for the pressure wound.
I replied to SA Ambulance and included ‘FYI. The pressure sores continue to be a problem, and I continue to get treatment. Just in case that was relevant to the complaint’.
Shortly following this I received another email that clarified a number of points. The SA Ambulance has achieved accreditation and one of the requirements is to maintain a commitment to the ongoing education of our staff in pressure sore prevention. They mentioned a few other points, and I was satisfied that everything was in place to prevent pressure injury. The paramedics that took me to the hospital just made a mistake, and they received further training. The email also made mention of my pressure sore and again apologised for the incident. Now happy that the matter has been addressed by SA Ambulance and now the healing continues.
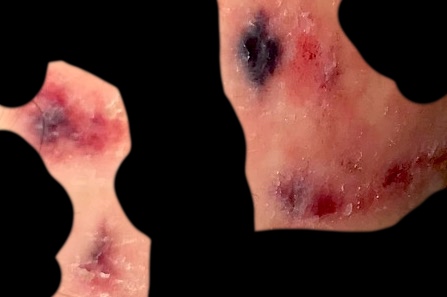
Images of my pressure sores
As the sore is almost healed, I gave the invoice for the ambulance ride to my health insurance for payment. I’ve included two photos below, and for your benefit, have hidden as much of my skin as possible :-). Hope the images motivate you to take action with pressure sore prevention.

After 14 weeks, the dressings have ceased, and in the 15th week, I returned to the pool. The RDNS continue to visit on a weekly basis to monitor the healing of the damage.
Pressure sore prevention is much better than the cure. Possibly pressure sores cause you pain, click here for a blog about dealing with pain.